Pelvic organ prolapse is something that happens to women. There is increased risk of pelvic organ prolapse for women who have had their children via vaginal delivery. However chronic cough, straining to empty the bowel, heavy lifting and being over your ideal weight, can all increase risk of pelvic organ prolapse. In other words, you can get prolapse even if you have not had a baby.
So what is pelvic organ prolapse?
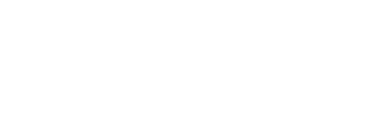
Pelvic organ prolapse is where one, two, or even three major pelvic organs drop down towards vaginal entrance. The prolapse can then progress below the vaginal entrance. If you look at the diagram below, you will see that the bladder sits in front of the vagina; the uterus sits above the bladder (in some people it sits back and is called “retroverted” uterus); the rectum, ie the lower part of the bowel, sits behind the vagina. The bladder can fall forward pushing down on the vaginal wall at the front. The uterus can fall down from above into the vagina and towards the vaginal entrance. The rectum can push from behind onto the back vaginal wall. There are several terms that are used to describe prolapse: bladder prolapse can be called “anterior wall prolapse” or “cystocoele”. Uterus prolapse can be called “uterine descent”. Rectum prolapse can be called “posterior wall prolapse” or “rectocele”. If a women has had a hysterectomy with removal of the cervix, the top of the vagina can still prolapse later on. This is called “vault prolapse”.
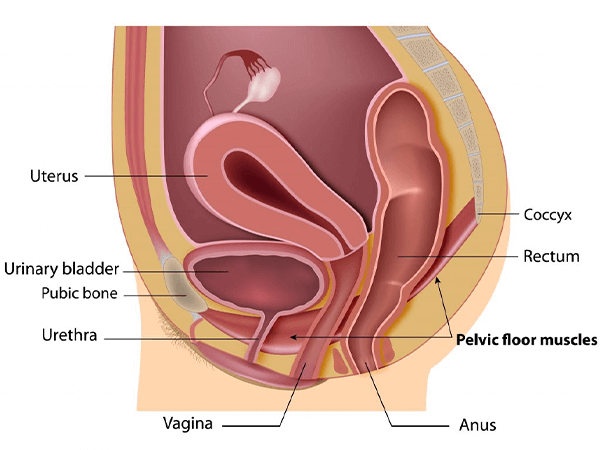
The following diagram demonstrates prolapse of the posterior vaginal wall.
In this diagram, the rectum is pushing the back wall down and it is bulging out of the vaginal entrance. The same can happen with uterus from above or bladder from in front.
How is prolapse measured?
All medical practitioners working with people with prolapse use a scale which measures the prolapse above and below the level of vaginal entrance. There are four “stages” of prolapse:
- stage 1 = prolapse stays well above level of vaginal entrance
- stage 2 = prolapse comes to 1cm above to 1cm below the entrance
- stage 3 = prolapse comes more than 1cm below the vaginal entrance
- stage 4 = prolapse is right out far as it can descend.
How do I know if I have prolapse?
Firstly, certain vaginal deliveries carry extra risk for prolapse:
- delivery of large baby more than 4 kgs (9lbs)
- pushing phase (second stage of labour) more than an hour and a half
- forceps assisted delivery
- 3rd degree tear i.e. tear towards and into the back passage.
if you have had any of these factors during a delivery, please work very hard on your pelvic floor exercises for life! If you have had any of these factors, you may have some prolapse but not know it. It is important to do the right thing to prevent it becoming a problem as life goes on.
Many women start to notice a heavy pelvic sensation, or a dragging feeling within the vagina. Some don’t have any sensation that anything is wrong. However they might notice a bulge at the vaginal entrance when showering or wiping. Some women notice a bulge after emptying the bowel. As soon as you have any concern about prolapse you can still do something about it. It is not too late. Ideally all women would do pelvic floor exercise regularly through life but life is not always ideal. We don’t always do what is ideal! But remember, it is never too late to get started.
What can I do about prolapse?
Pelvic floor exercise!!!
Ideally, as mentioned above, we would all be taught to do pelvic floor exercises early in life. Unfortunately, it is a fact that lots of people who read about how to exercise may not get it right. Even those who are told how to exercise might not get it right. So at least one assessment with a health professional at some stage of life would be great.
If you start to have symptoms of prolapse, start exercising pelvic floor AND most importantly, learn to USE the muscles in daily activities. Activities which put pressure in the abdomen above the pelvis tend to cause prolapse. So, you must try and learn to tighten pelvic floor when you
- cough
- sneeze
- laugh
- lift
- push
- pull
- exercise
- especially impact exercise or abdominal exercises like crunches and leg lifts.
Will I need surgery?
Lots of women do go on to have successful surgery. Lots of women also start doing exercises and find they are comfortable so don’t need to go on to surgery. Nowadays, since the recent controversy over vaginal mesh repair for prolapse, most Gynaecologists will suggest that you at least start a program of exercise first and review after a certain period. That way, at least you know you have prepared yourself mentally for surgery. You will know that you did everything you could and that surgery needed to go ahead. There are also pessaries made of silicone which sit in the vagina and hold the prolapse back for those that don’t want surgery but want to try something to make them comfortable immediately. See the blog on “pessaries for prolapse” for more information.
What do I do now?
If you are worried that you have prolapse, come and see a Pelvic Floor Physiotherapist for assessment and to find out how to exercise correctly. If you see your G.P., you may be referred to a Gynaecologist who will most likely refer to Physio before going ahead with surgery. Your G.P. might send you for a pelvic ultrasound. Feel free to ask to speak to the Physio at any stage for advice. Make contact with our contact page here at PPFP.